Care Neighborhood Enhanced Case Management
Care Neighborhood Enhanced Case Management (ECM) is our intensive case management program that helps high-risk, high needs patients connect to local community resources and prevent unnecessary hospitalizations by focusing on addressing the social determinants of health.
How do we do it? 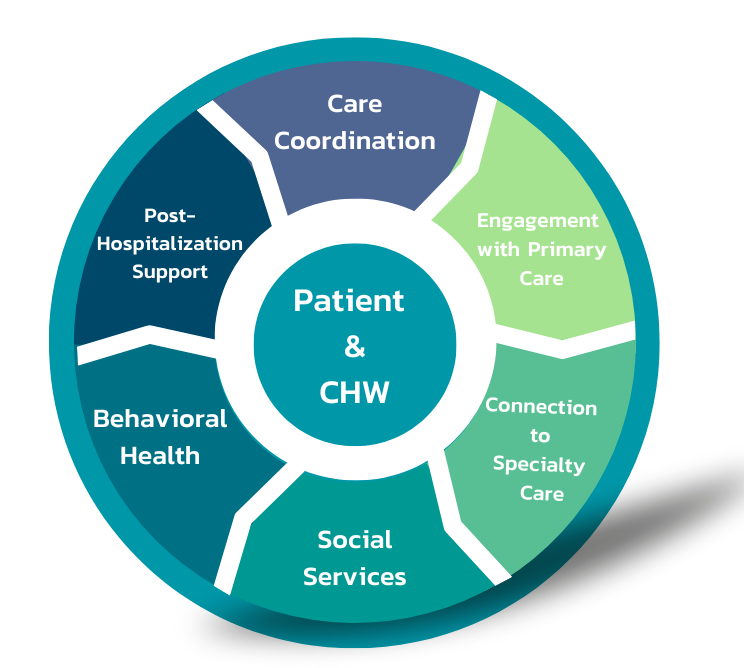
CHCN partners with MediCal managed plans in Alameda County. These partners currently administer the Enhanced Care Management program that funds Care Neighborhood ECM as part of California’s CalAIM initiative. Patients that have complex medical and social issues are identified by multiple entities. Patient information is collected to determine eligibility based on the criteria put forth by DHCS. A patient’s eligibility is made visible in the electronic health record (EHR) OCHIN Epic. Community Health Workers (CHWs) at our eight federally qualified healthcare centers use this data to outreach to patients and offer them ECM services.
CLICK TO READ MORE
CHWs get to know their patients one-on-one and assess their medical, behavioral, and social needs. After identifying their needs, the CHW collaborates with the patient to create a patient-centered Care Plan. CHWs and patients work together on the goals in their care plan that the patient has identified as a priority. The patient’s care plan is reviewed by the CHW, patient, CN central team, and members of the clinic staff on a quarterly basis to ensure goals remain relevant to the patient’s changing needs. All patient goals align with various social determinants of health, such as housing, transportation, and medical goals. CHWs meet their patients in the clinic, hospital, home or in the community depending on the patient’s needs and preferences. The ultimate goal is to support patients with obtaining the resources needed to address their health and wellness goals and empower them to be able to independently use these resources after the patient has graduated from the program.
CHCN’s CN Central staff includes a medical doctor, social workers, a nurse, lead CHW, operations manager, and a program coordinator who provide training, technical support and clinical support in the field.
CHCN’s data team supports the program with billing and tracking data through various data systems including Tableau and Structured Query Language (SQL).
Delivering Results
CHCN’s Care Neighborhood ECM approach has demonstrated positive returns on investments including decreased hospital re-admission rates, improved use of integrated behavioral health, decreased ER use and increased primary care visits. With ongoing support from our health plan partners we have over 55 CHWs in our 8 community health center organizations who currently serve over 1,000 patients in total. Care Neighborhood ECM continues to successfully demonstrate total cost of care savings per member per month. CHCN is the largest ECM provider in Alameda County.
Technology & Data Analytics
Care Neighborhood ECM has partnered with OCHIN Epic to create a specialized case management platform integrated in the EHR. On the case management platform, CHWs can review who they are working with, who is eligible for enrollment, and which of their enrolled patients are hospitalized. The case management platform also allows CHWs to view patient’s records, document encounter notes, care plan goals, and assessment results. All the work done by CHWs within the case management platform is also visible to other clinic staff which provides opportunities for interdepartmental collaboration in patient care.
CLICK TO READ MORE
Care Neighborhood ECM also uses Tableau, a data visualization program, to present Care Neighborhood’s ECM progress and impact. Tableau pulls data from Epic to demonstrate the growth of Care Neighborhood ECM over time and progress with the Care Neighborhood ECM eligible population on an individual CHW level and a larger programmatic level. CHWs can also use Tableau to monitor their outreach and enrollment metrics, allowing for more effective caseload management.
Care Transition when patients are hospitalized
A core function of the Care Neighborhood ECM program is to prevent hospitalizations by addressing the social determinants of health. Supporting patients during and immediately following a recent hospitalization is an essential part of this process. Using internal data analytics tools, the Care Neighborhood ECM clinical team tracks patients in the program who have been admitted to a local hospital. Using this information, we can proactively coordinate with hospitals to ensure effective discharge planning for our patients. CHWs also help their patients connect with the appropriate resources when they leave the hospital. The Care Neighborhood ECM nurse works closely with the CHW post-hospitalization to ensure smooth follow-up and get patients back into Primary Care. At the health care center, with support from Care Neighborhood ECM staff, the Community Health Worker, Social Worker, and Nurse review the patient’s hospital stay and consider ways to support their patient in preventing future hospitalizations.
For inquiries please reach out to the Enhanced Case Management Team: cnsupport@chcnetwork.org
CHWs are hired directly by their health centers and are ideally from the community they serve.
Community health worker training